Case Report Volume: 1 Issue:1
Abstract
Background: Managing lower extremity osteomyelitis remains a significant clinical challenge. Although surgical resection of infected bone offers definitive treatment, it often results in substantial osseous defects and altered biomechanics - especially concerning when the calcaneus, the primary weight-bearing tarsal bone, is involved.
Case Presentation: We present the case of a 64-year-old female who developed calcaneal osteomyelitis following a corticosteroid injection administered for plantar fasciitis. This report highlights the often-overlooked risks associated with corticosteroid injections in the treatment of plantar fasciitis and describes the successful management of calcaneal osteomyelitis using an antibiotic coated intraosseous rod.
Results: Bone biopsies positive for acute osteomyelitis of the right talus and calcaneus and septic arthritis of the ankle. Imaging and histopathologic data support the calcaneus as the initial site of infection, with subsequent contiguous spread to the talus and ankle joint. Successful resolution of infection was achieved through arthroscopic debridement and washout of the ankle, Masquelet technique, and insertion of an antibiotic coated intraosseous rod. Definitive fixation included a tibiotalocalcaneal arthrodesis nail.
Keywords: calcaneal osteomyelitis, plantar fasciitis, corticosteroid injection, antibiotic rod, masquelet technique, limb salvage, tibiotalocalcaneal arthrodesis
Abbreviations
CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; MRSA, methicillin-resistant Staphylococcus aureus; MRI, magnetic resonance imaging; CT, computed tomography
Introduction
Plantar fasciitis is a common foot disorder accounting for about one million physician visits per year.1 When conservative treatments fail, corticosteroid injections are frequently employed for symptom relief and have demonstrated clinical efficacy.1,2 However, despite their widespread use, these injections carry risk of complications including infection, particularly if aseptic protocols are not followed.3 Although reported complications from corticosteroid injections for plantar fasciitis are rare, Wronka et al. documented a case of acute calcaneal osteomyelitis following corticosteroid administration despite adherence to aseptic technique.3 We present a similar case involving a 64-year-old female who was diagnosed with acute osteomyelitis of the calcaneus and talus after administration of a corticosteroid injection for plantar fasciitis. Calcaneal osteomyelitis accounts for approximately 3-10% of all bone infections and may result from hematogenous spread, trauma, chronic ulceration, or iatrogenic causes.4,5 Treatment of calcaneal osteomyelitis poses distinct challenges. The calcaneus bears 50-60% of the body weight during ambulation, and the overlying soft tissue has limited vascularity, making wound coverage and healing difficult.5 Multiple studies describe the successful treatment of lower extremity osteomyelitis with long-term antibiotic therapy, debridement, partial or total calcanectomy, and even below the knee amputation in refractory cases.5-7 This case report presents a staged surgical approach incorporating an intraosseous, antibiotic coated rod to effectively treat the infection while preserving limb function, offering a novel limb-salvage strategy in a challenging anatomical context.
Case report
A 64-year-old female presented to our institution with a right foot infection following a corticosteroid injection administered to the right heel for plantar fasciitis. The patient reported receiving a corticosteroid injection to the plantar fascia within a six-week period prior to developing symptoms. These injections were administered at an outside facility, and while the specific dosage and steroid type were not available, no other inciting trauma or invasive procedures were identified. Following the injection, the patient developed progressive pain, erythema, and swelling localized initially to the right plantar heel, suggesting the calcaneus as the primary site of infection. Prior to presentation, she had been hospitalized at another facility, where multiple bone biopsies confirmed acute osteomyelitis involving the talus and calcaneus. Laboratory results revealed significantly elevated inflammatory markers, with a C-reactive protein (CRP) of 185 mg/dL and erythrocyte sedimentation rate (ESR) of 39 mm/hr.
Bone cultures were positive for methicillin-resistant Staphylococcus aureus (MRSA).
Initial management included prolonged intravenous antibiotic therapy with daptomycin and ceftaroline, in addition to multiple surgical interventions, including incision and drainage, bone biopsies, and dorsolateral fasciotomy for suspected compartment syndrome. Upon transfer to our facility, the patient reported moderate pain and exhibited erythema and edema over the dorsolateral aspect of the right ankle (Figure 1). Repeat laboratory studies demonstrated persistently elevated inflammatory markers (ESR 85 mm/hr, CRP 5.0 mg/dL).

Figure 1 Clinical presentation showing erythema to the dorsal lateral ankle and rearfoot, and diffuse non-pitting edema to the right foot and ankle.
Plain radiographs were inconclusive. Magnetic resonance imaging (MRI) with contrast revealed heterogeneous bone marrow signals consistent with osteomyelitis. Computed tomography (CT) imaging showed scattered hyperdense areas and a moth-eaten appearance in both the talus and calcaneus (Figure 2). Blood cultures at the time of admission were negative. Pathological analysis confirmed septic arthritis of the ankle joint and persistent acute osteomyelitis of the talus and calcaneus. The radiologic and clinical findings suggested contiguous spread from the calcaneus to the talus and ankle joint, likely through the subtalar joint, a recognized anatomic pathway for infection progression in the hindfoot.
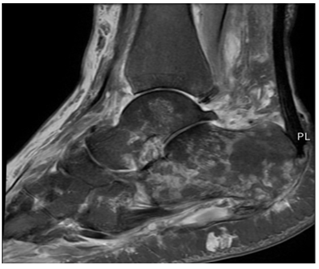
Figure 2 CT scan of right foot showing scattered areas of hyperdensity in the talus and calcaneus with a moth-eaten appearance.
The patient subsequently underwent a staged surgical reconstruction. Stage one included the application of a multiplanar external fixator, arthroscopic joint washout, and insertion of an antibiotic coated intraosseous calcaneal rod, along with a tibiotalocalcaneal antibiotic coated rod. A second-stage procedure was planned to replace the temporary rods with a definitive tibiotalocalcaneal arthrodesis nail.
Results
The patient underwent successful two stage surgical reconstruction for infection control and limb salvage. Stage one included application of a multiplanar external fixator, arthroscopic ankle joint washout, and placement of an antibiotic coated intraosseous calcaneal rod along with a tibiotalocalcaneal antibiotic coated rod. The antibiotic coated intraosseous calcaneal rod was made from a 50 mm threaded rod coated with poly methyl methacrylate mixed with 1 gram of vancomycin and 1 gram of gentamicin. The antibiotic coated tibiotalocalcaneal rod was made from a 150 mm threaded rod with multiple nuts for stability and a distal hinge for later extraction. The rod was also coated with poly methyl methacrylate mixed with 1 gram of vancomycin and 1 gram of gentamicin (Figure 3). The area of bone was reamed and irrigated prior to antibiotic coated rod insertion (Figure 4).

Figure 3 Intraoperative image demonstrating an antibiotic-coated rod.
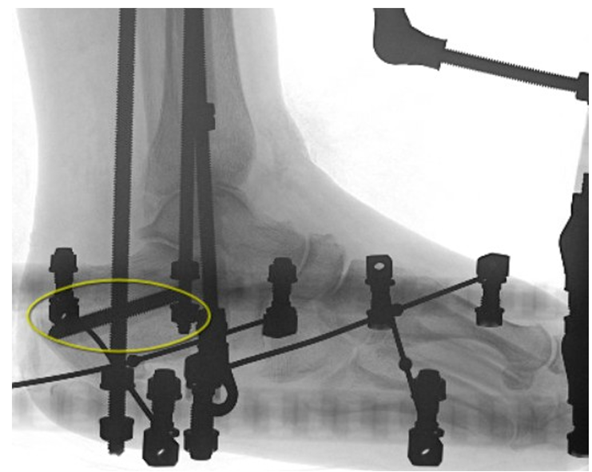
Figure 4 Lateral radiograph of the right foot demonstrating placement of an antibiotic-coated intraosseous rod within the calcaneus. The radiopaque cement surrounding the rod reflects polymethyl methacrylate mixed with vancomycin and gentamicin, used for local antibiotic delivery and induction of membrane formation as part of Masquelet technique.
After 68 days, stage two was performed involving removal of external fixator, removal of drug delivery devices, and insertion of definitive tibiotalocalcaneal arthrodesis nail. Routine monthly radiographs and repeat inflammatory markers were followed. At the time of the second stage, inflammatory markers improved significantly with ESR reduced to 32 mm/hr and CRP to 6 mg/dL. Radiographic evidence of bony fusion across the ankle and subtalar joints was observed 61 days following stage two (Figure 5). The patient progressed to partial weight bearing at 26 days post-operatively. At final follow-up, all surgical wounds were fully healed, with no recurrent signs of infection or hardware complications.
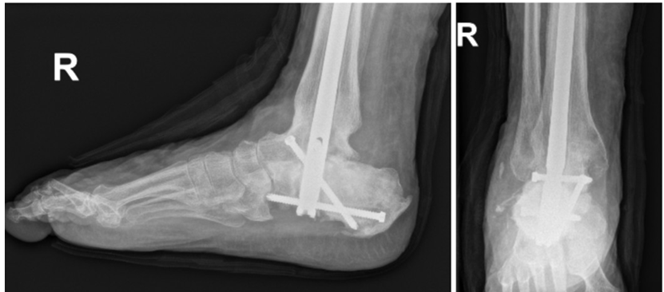
Figure 5 Foot and ankle radiographs demonstrating tibiotalocalcaneal fusion with use of an intramedullary nail at 12 month follow-up.
Discussion
Corticosteroid injections are a commonly utilized treatment for plantar fasciitis, offering effective symptom relief. However, although generally considered safe, these injections are not without risk. Rare but serious complications such as acute calcaneal osteomyelitis can occur, particularly if bacterial contamination is introduced in the process.3 In our case, the patient received a corticosteroid injection to the plantar fascia at an outside facility. Although the exact dosage was unavailable, the close correlation between the injection and the development of localized heel pain, swelling, and erythema over the plantar aspect strongly suggests the calcaneus as the initial site of infection. The calcaneus is the largest tarsal bone and plays a crucial role in weight bearing, absorbing approximately 50-60% of the body weight during ambulation. Calcaneal osteomyelitis presents a significant clinical challenge due to its biomechanical importance and carries a high risk of disability, and in some cases may lead to systemic infection.4 Surgical management often involves aggressive debridement and resection of infected portions of bone, but this can result in large osseous defects with devastating effects on biomechanics.5,6
In our case, the infection was initially isolated to the calcaneus, with subsequent spread to the talus and ankle joint. The progression of infection likely occurred through contiguous extension through the subtalar joint, a common anatomic route of communication between these bones. Septic arthritis of the ankle joint confirmed further spread, likely followed by cortical destruction and joint involvement.
The Masquelet technique describes a two stage approach of managing large bony defects using the concept of induced membrane.8 Many studies have described successful treatment of lower extremity osteomyelitis using the Masquelet technique with antibiotic impregnated cement.9,10 Our case report showcases the successful treatment of calcaneal osteomyelitis using an antibiotic coated intraosseous rod through local elution of antibiotics to surrounding soft tissue and bone. This technique avoided the morbidity associated with calcanectomy or below knee amputation and ultimately preserved the patient’s limb and biomechanics.
Conclusion
This case illustrates a rare but severe complication of corticosteroid injection for plantar fasciitis - calcaneal and talar osteomyelitis. It emphasizes the importance of early recognition and intervention when infectious complications arise. Our staged approach using local antibiotic delivery through intraosseous antibiotic coated rods and external fixation offers a viable limb-salvage strategy in the setting of complex hindfoot infections. At over one year follow-up, this approach was able to provide the patient with a limb salvage option with minimal resection of non-articular bone. Surgeons managing similar cases should consider a multidisciplinary, stepwise protocol to optimize source control, preserve biomechanical integrity, and ultimately improve patient outcomes.
Acknowledgements
The authors thank all the participants for their efforts in responding to the scales as well as the editors of this periodical for their constructive comments.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Tatli YZ, Kapasi The real risks of steroid injection for plantar fasciitis, with a review of conservative therapies. Curr Rev Musculoskelet Med. 2009;2(1):3‒9.
- Wronka KS, Sinha Calcaneal osteomyelitis following steroid injection for plantar fasciitis: a case report. Foot Ankle Spec. 2012;5(4):253‒255.
- Holland C, Jaeger L, Smentkowski U, et al. Septic and aseptic complications of corticosteroid injections: an assessment of 278 cases reviewed by expert commissions and mediation boards from 2005 to 2009. Dtsch Arztebl Int. 2012;109(24):425‒430.
- Merlet A, Cazanave C, Dauchy FA, et Prognostic factors of calcaneal osteomyelitis. Scand J Infect Dis. 2014;46(8):555‒560.
- McCann MJ, Wells Calcaneal Osteomyelitis: Current Treatment Concepts. Int J Low Extrem Wounds. 2020;19(3):230‒235.
- Sabater-Martos M, Sigmund IK, Loizou C, et al. Surgical Treatment and Outcomes of Calcaneal Osteomyelitis in Adults: A Systematic J Bone Jt Infect. 2019;4(3):146‒154.
- Waibel FWA, Klammer A, Götschi T, et al. Outcome After Surgical Treatment of Calcaneal Osteomyelitis. Foot Ankle Int. 2019;40(5):562‒567.
- Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. 2010;41(1):27‒37.
- Conway JD, Elhessy AH, Galiboglu S, et al. Efficacy of Infection Eradication in Antibiotic Cement-Coated Intramedullary Nails for Fracture-Related Infections, Nonunions, and Antibiotics (Basel). 2022;11(6):709.
- Conway J, Mansour J, Kotze K, et Antibiotic cement-coated rods: an effective treatment for infected long bones and prosthetic joint nonunions. Bone Joint J. 2014;96-B(10):1349‒1354.

